“Practices using Outsourced Medical Billing Services often see collections increase by 20–30%.”
Outsourced Medical Billing Services are transforming the healthcare industry in 2025. While patient care remains the heart of every practice, denials, shrinking reimbursements, and compliance demands are quietly eroding practice revenue. Providers are working harder than ever but taking home less—because the money they’ve earned is trapped in billing errors, delayed claims, and inefficient processes.
We call this the Hidden Revenue Crisis. And it’s costing providers far more than they realize.
The Key to Smarter Practice Growth in 2025
Outsourced Medical Billing Services in 2025: A Smarter Choice for Providers
Medical Billing Services are no longer optional in 2025—they’re essential. The healthcare industry is standing at a financial crossroads. While patient care remains the heart of every practice, denials, shrinking reimbursements, and compliance demands are quietly eroding revenue. Providers are working harder than ever but taking home less—because the money they’ve earned is trapped in billing errors, delayed claims, and inefficient processes.
We call this the Hidden Revenue Crisis. And it’s costing providers far more than they realize.
The healthcare industry is standing at a financial crossroads in 2025. While patient care remains the heart of every practice, denials, shrinking reimbursements, and compliance demands are quietly eroding practice revenue. Providers are working harder than ever but taking home less—because the money they’ve earned is trapped in billing errors, delayed claims, and inefficient processes.
“The Ashez Group specializes in Outsourced Medical Billing Services tailored to psychiatry, ABA, dermatology, and labs.”
💡 How Much Money Are Providers Really Losing?
The numbers tell the story:
- 15–30% of revenue is lost every month due to billing inefficiencies.
- 90% of denials are preventable, but most practices don’t have the bandwidth to fix them.
- 1 in 5 claims is underpaid by payers, often without providers noticing.
- A/R beyond 45 days is the norm for many practices, instead of the exception.
What does that mean in dollars? For a small practice billing $100,000/month, even a 15% loss equals $15,000 left on the table. Over a year, that’s $180,000 in missed revenue—enough to hire staff, expand services, or invest in growth.
🔍 Why the Revenue Crisis Is Worsening in 2025
The challenges providers face aren’t new—but they’ve intensified.
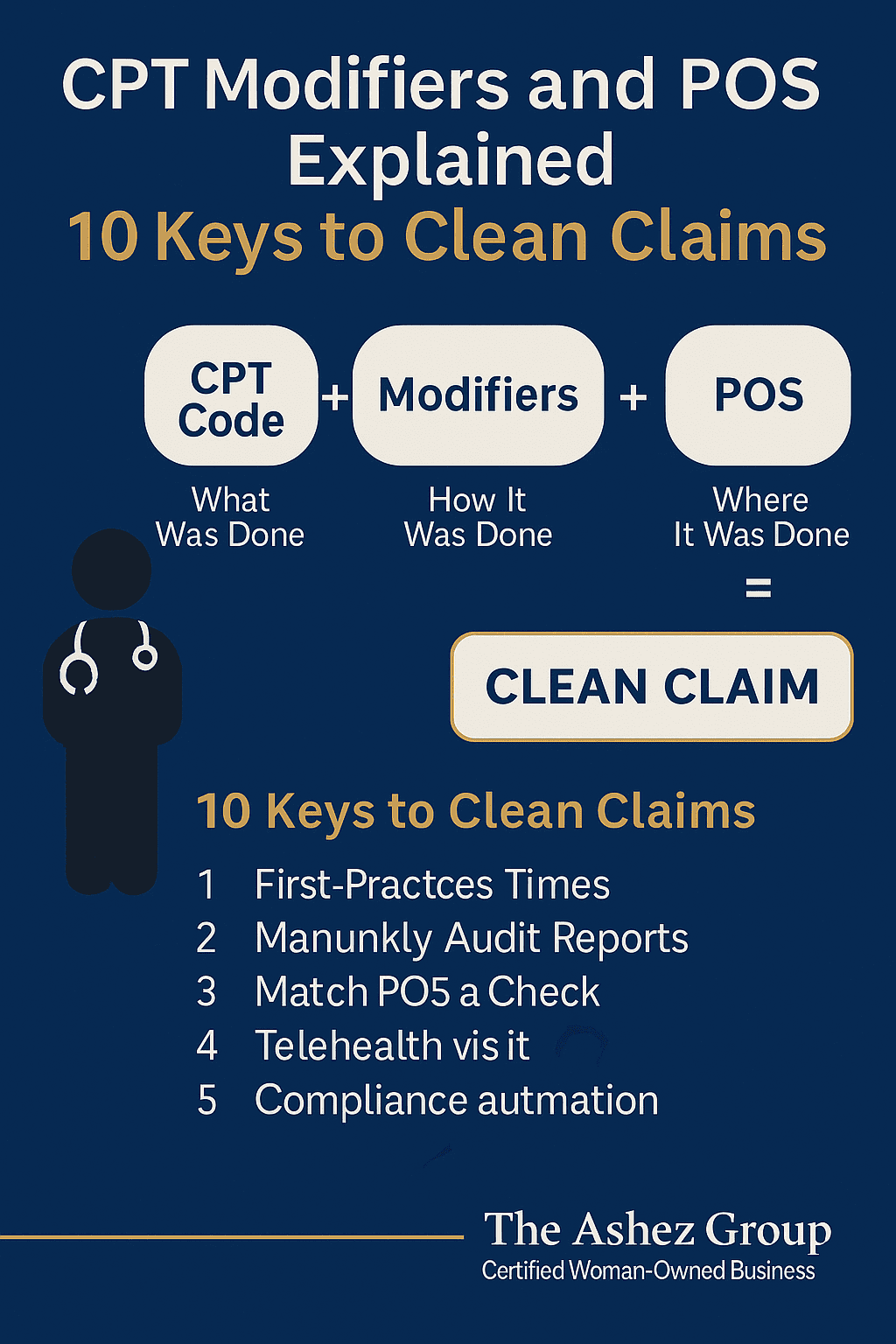
- Constant Payer Policy Changes
New rules, pre-authorization requirements, and coding changes are rolled out so frequently that staff can’t keep up. Miss one update, and your claim is denied. - Staff Shortages and Burnout
The post-pandemic workforce shortage is real. Billing staff are stretched thin, balancing multiple roles, which leads to errors and slower claim submission. - Compliance and Regulatory Pressures
HIPAA, CMS, Medicare, and Medicaid have increased oversight. A single mistake can lead to audits or penalties. - Outdated Technology
Many practices still rely on older EHR and billing systems that can’t handle today’s claim complexity. Manual work = slower processes = lost revenue.
🚀 The Smarter Solution:
The answer isn’t to make providers and staff work harder. It’s to work smarter. That’s why more practices are outsourcing billing to expert partners like The Ashez Group.
Here’s what happens when you do:
- ✅ 20–30% increase in collections
- ✅ Faster reimbursements through clean claim submission
- ✅ Denial prevention with proactive rules tracking
- ✅ Lower overhead compared to in-house billing teams
- ✅ Specialty-specific expertise for psychiatry, ABA, dermatology, labs, dental, and more
- ✅ Compliance protection with HIPAA, CMS, and payer regulations
Outsourcing isn’t just about billing—it’s about protecting the financial health of your practice.
📊 Case Study: Results After Using The Ashez Group Medical Billing Services
“After partnering with The Ashez Group for outsourced medical billing services, a mid-sized behavioral health practice reduced denials by 40% in just 90 days.”
- Denials above 18%
- A/R averaging 60+ days
- Overwhelmed staff spending more time on claims than patients
Within just 90 days, results changed dramatically:
- 📉 Denials reduced by 40%
- 💵 Collections increased by 22%
- ⏱️ A/R dropped to under 30 days
This allowed the providers to re-focus on patient care, while The Ashez Group ensured every earned dollar was collected.
🏆 Why Providers Trust The Ashez Group
We’re not just a billing company—we’re a certified woman- and minority-owned partner committed to your success.
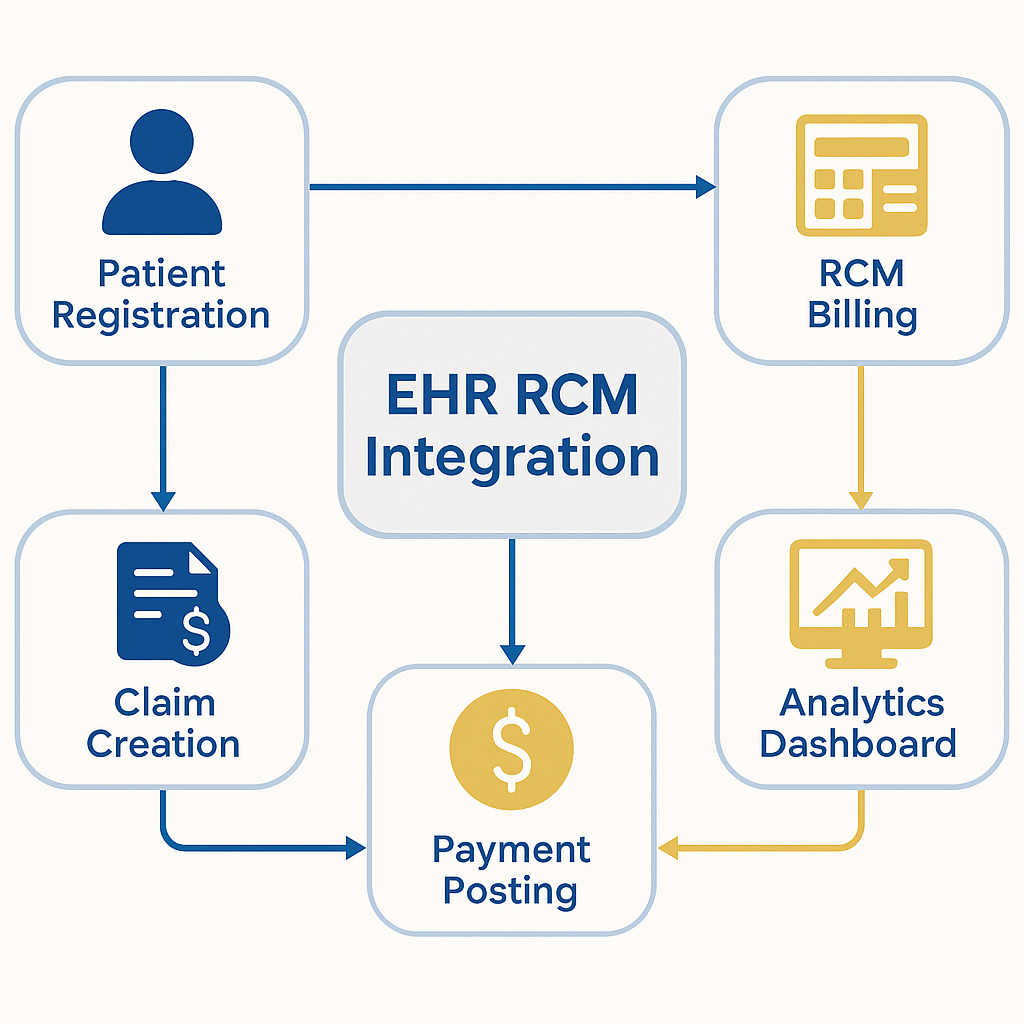
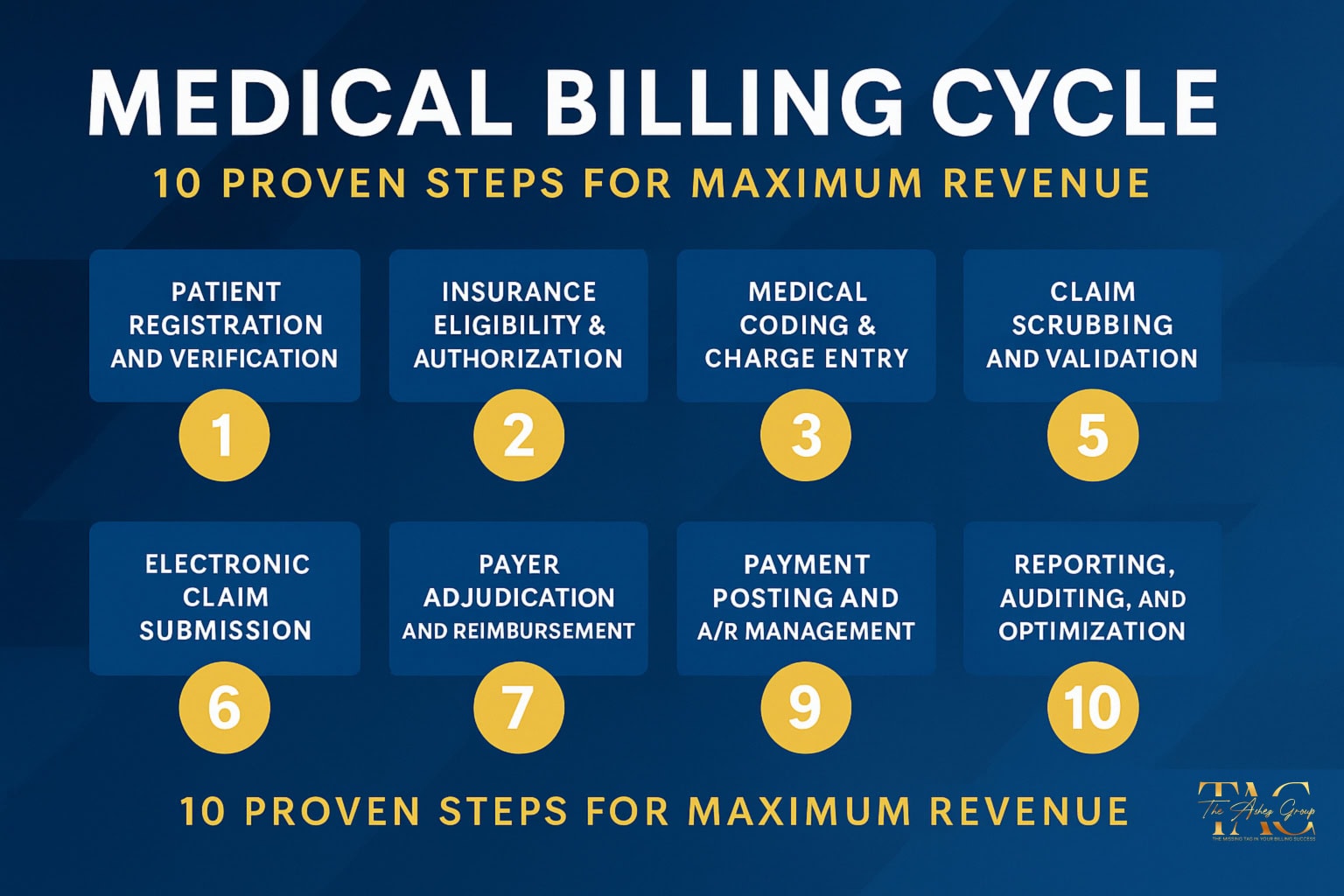
Our services cover the entire revenue cycle:
- Medical Billing & Coding
- Revenue Cycle Management (RCM)
- Denial Management & A/R Recovery
- Credentialing & Enrollment
- Virtual Front Desk & Admin Support
- Practice Growth Consulting
With transparent pricing, customized solutions, and a team of certified billing specialists, we deliver more than services—we deliver peace of mind.
❓ Frequently Asked Questions (FAQ)
Q: Why should I outsource medical billing in 2025?
A: Outsourcing reduces denials, improves cash flow, and cuts costs compared to in-house billing.
Q: What types of practices benefit most?
A: Psychiatry, ABA therapy, dermatology, labs, primary care, and dental practices see strong ROI.
Q: How quickly can outsourcing improve my revenue?
A: Many practices see improvement within 60–90 days.
Q: Is outsourcing secure?
A: Yes. At The Ashez Group, we’re HIPAA-compliant, follow CMS guidelines, and maintain the highest standards of patient data protection.
📈 The Bottom Line: Don’t Wait to Protect Your Revenue
The Hidden Revenue Crisis is costing providers money every single day. If your practice has rising denials, delayed A/R, or staff stretched too thin, now is the time to rethink your billing strategy.
📞 Call us today: 844-824-4040
📧 info@theashezgroup.com
🌐 www.theashezgroup.com
👉 “Contact The Ashez Group today to learn how our Outsourced Medical Billing Services can safeguard your revenue.”
The Ashez Group – The Missing TAG in Your Billing Success
AAPC (coding & billing authority) → AAPC: Understanding Denials
AMA (medical coding & compliance) → AMA CPT® Updates
CMS (Medicare/Medicaid rules) → CMS Billing Guidance