Behavioral health complex billing is one of the most misunderstood, high-risk, and denial-prone areas in medical billing and revenue cycle management (RCM). Unlike traditional medical billing, behavioral health billing involves a unique combination of time-based therapy codes, strict documentation requirements, specialized modifiers, provider supervision rules, coverage restrictions, and payer-specific compliance regulations. As behavioral health demand continues to grow in 2026—driven by mental health awareness, telehealth expansion, and workforce shortages—the complexity of billing also increases.
For RCM companies, billers, and medical practices, mastering behavioral health complex billing is no longer optional. It is essential for preventing revenue leakage, avoiding payer audits, ensuring compliance, and improving clean-claim rates. This in-depth guide explains every major element that billing professionals must know to succeed in this highly specialized area.
At The Ashez Group, a Certified Woman-Owned Medical Billing & RCM Company, we manage billing for psychiatrists, therapists, mental health NPs, psychologists, counselors, and multi-specialty behavioral practices across the U.S.
This guide breaks down everything an RCM team must know to succeed.
🔍 1. What Makes Behavioral Health Complex Billing So Complicated?

Behavioral health billing contains far more nuances than general medical billing. RCM teams must navigate:
✔ Time-based CPT billing
✔ Therapy-specific coding rules
✔ Modifier-heavy claims
✔ Supervision indicators (HP/HT)
✔ High-denial risk codes
✔ Cross-state telehealth laws
✔ Medicaid variation by state
✔ Frequent prior authorizations
✔ Documentation-specific criteria
✔ Credentialing limitations
Unlike general medical billing, where procedures are straightforward and documentation follows a simple clinical structure, behavioral health documentation must justify:
- Medical necessity
- Therapeutic interventions
- Time spent
- Risk assessment
- Clinical progress
- Behavioral indicators
This makes RCM workflows more complex and more prone to payer scrutiny.
📘 2. Key CPT Codes That Define Behavioral Health Complex Billing
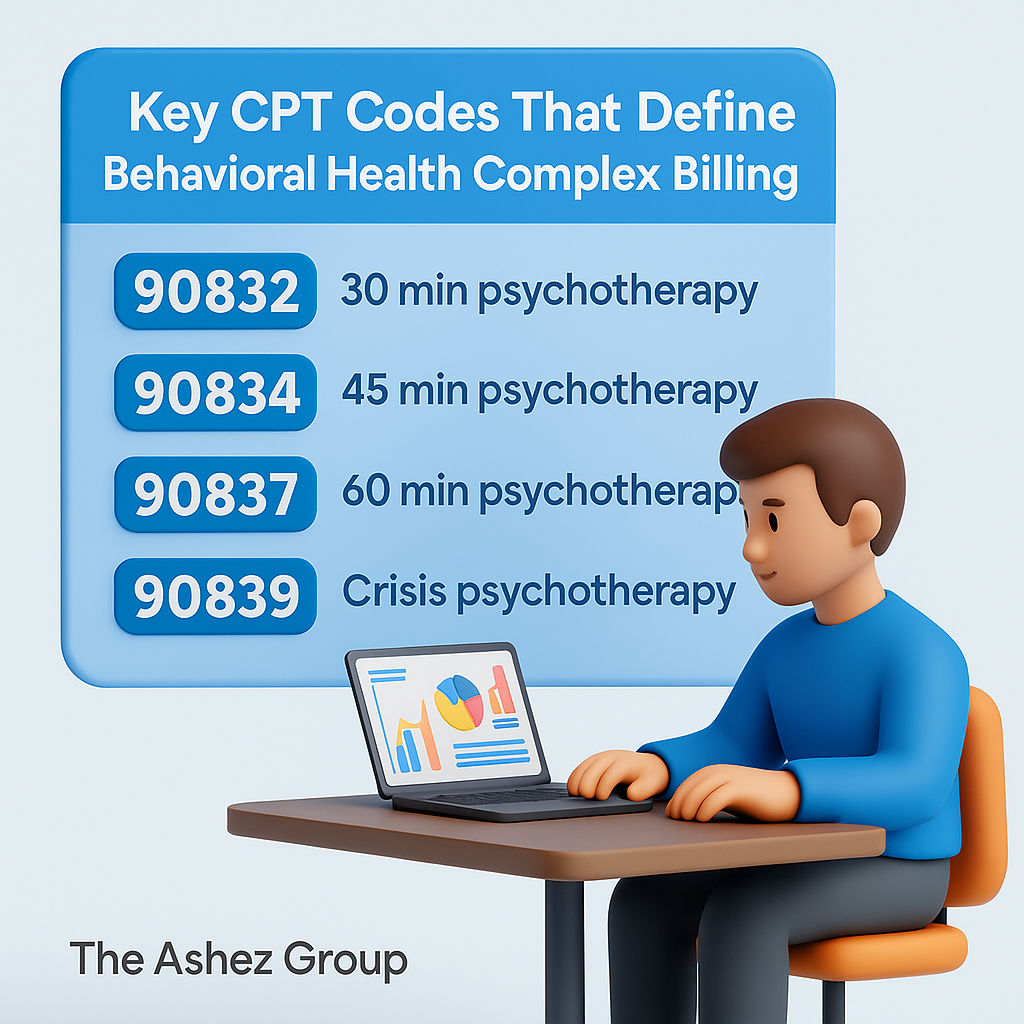
To succeed in behavioral health complex billing, billing professionals must master the CPT codes used across psychotherapy, psychiatry, evaluation, group therapy, and complex sessions.
A. Psychotherapy Codes (Time-Based)
These codes require accurate documentation of start and stop times, clinical interventions, and medical necessity:
- 90832 – 30-minute psychotherapy
- 90834 – 45-minute psychotherapy
- 90837 – 60-minute psychotherapy
- Most frequently denied due to medical necessity reviews
- 90846 / 90847 – Family psychotherapy
- 90853 – Group therapy
Behavioral health complex billing is heavily time-driven. Any mismatch between documented minutes and billed CPT code can lead to denials or audit risk.
B. Psychiatry / Medication Management Codes
Used by psychiatrists and psychiatric NPs:
- 90792 – Psychiatric diagnostic evaluation
- 99213 – 99215 – E/M medication management codes
These must follow E/M guidelines, plus mental status exam documentation.
C. Add-On Codes for Complex Cases
Used when sessions have additional complexity:
- +90785 – Interactive complexity
- +99354 / +99355 – Prolonged therapy
- +90863 – Pharmacological management add-on
Each add-on code has strict payer requirements and must be supported by documentation.
🧾 3. The Documentation Standards That Drive Behavioral Health Complex Billing
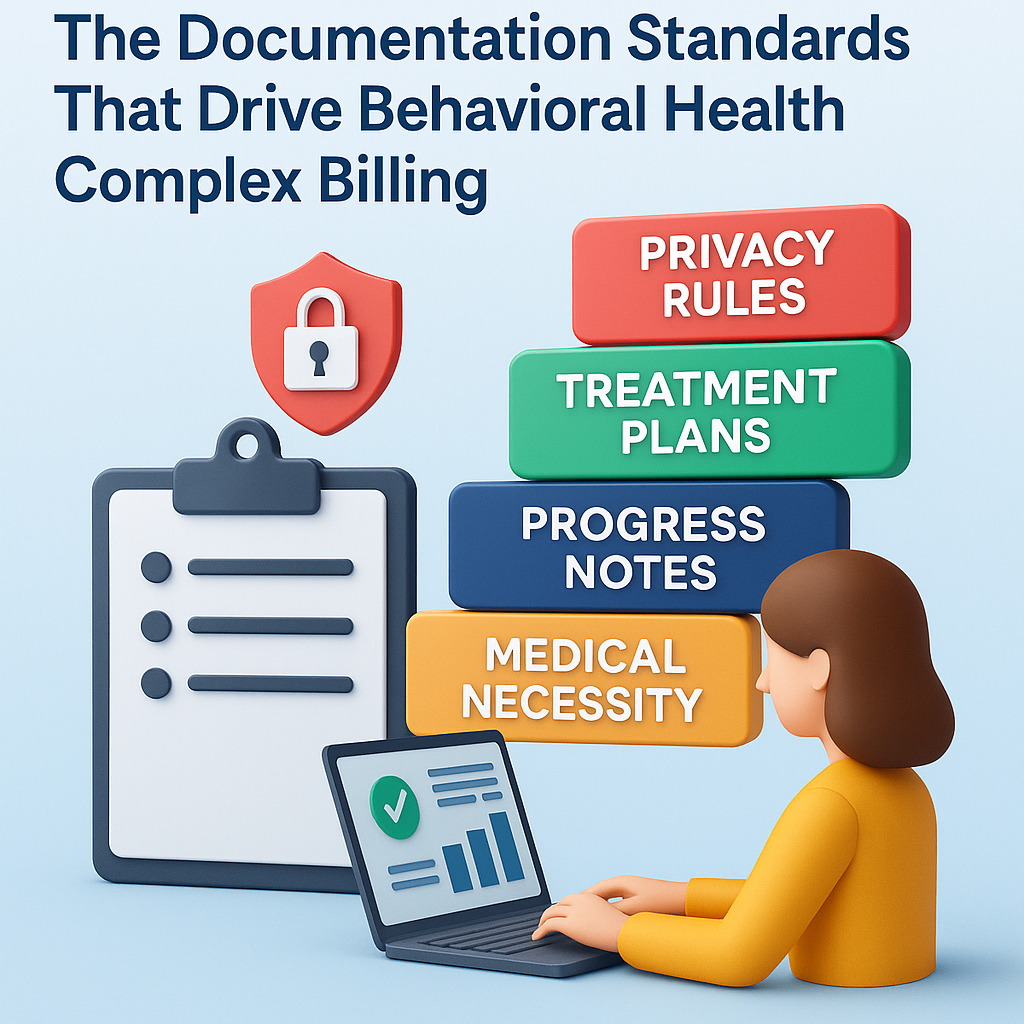
Behavioral health documentation is more detail-heavy than medical specialties because payers must validate:
- Time spent
- Interventions used
- Patient response
- Treatment plan progress
- Risk assessment
- Complexity indicators
- Crisis management
- Co-occurring conditions
To meet payer requirements, documentation must include:
✔ Start and stop time
✔ Type of therapy (CBT, DBT, EMDR, play therapy, etc.)
✔ Progress toward goals
✔ Medical necessity statements
✔ Patient behavioral observations
✔ Risk (SI/HI, substance use, crisis)
✔ Treatment plan alignment
✔ Interventions and response
Missing any of these creates denials, downcoding, or audit exposure.
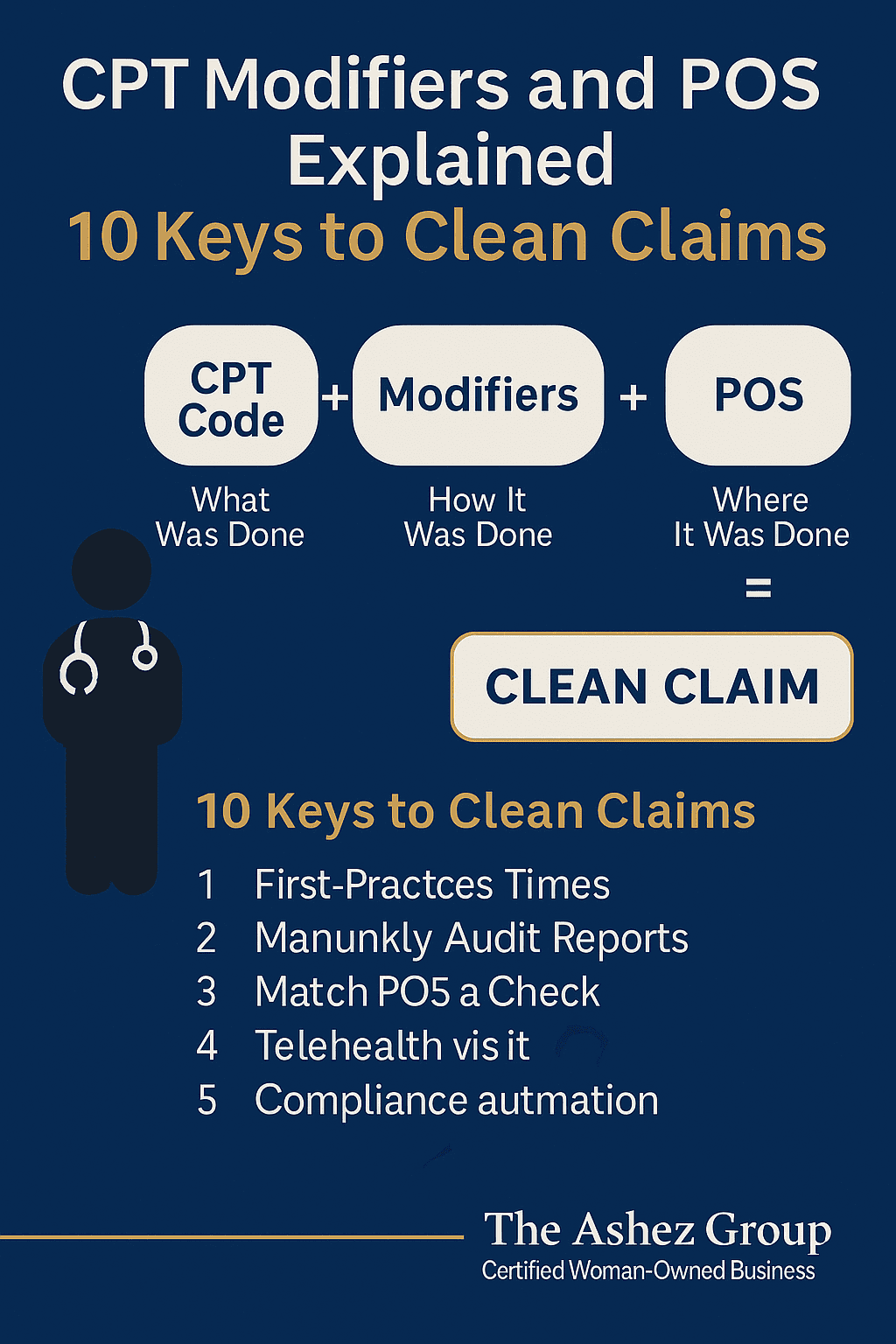
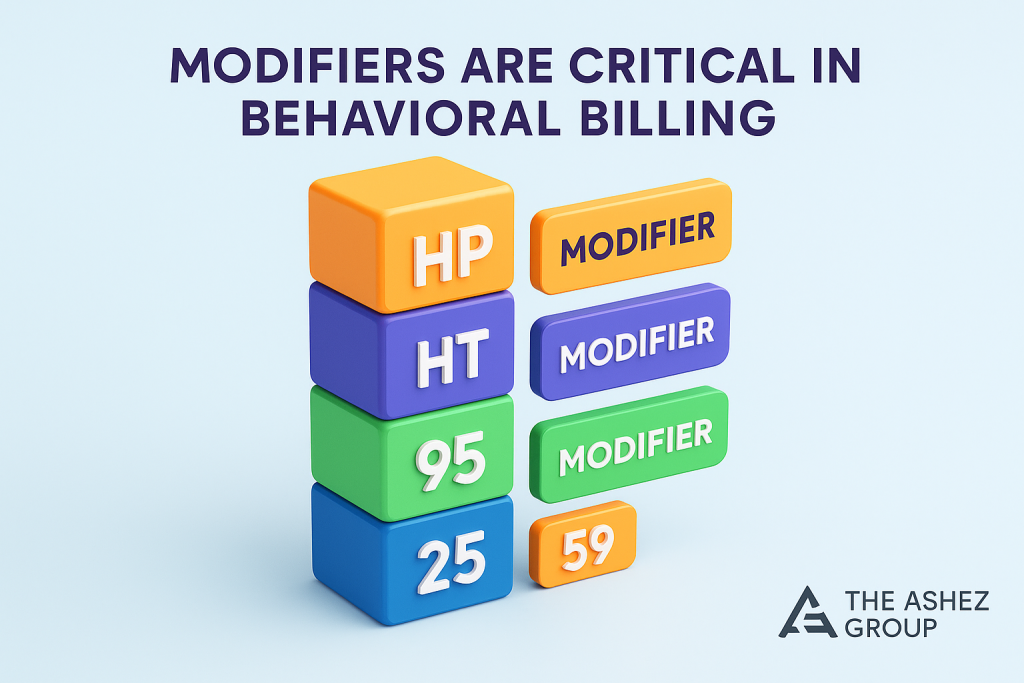
🎛️ 4. Modifiers Are Critical in Behavioral Health Complex Billing
Behavioral health billing uses a higher number of modifiers than most specialties. Incorrect or missing modifiers are a top cause of denied claims.
A. Telehealth Modifiers
- 95 — Synchronous audio/video
- GT — Telehealth via interactive audio/video
- FQ / FR — Audio-only or split services (state-specific)
B. E/M + Therapy Modifiers
- 25 — Significant, separate E/M + psychotherapy same day
- 59 — Distinct procedural service
These modifiers are essential when psychiatrists perform medication management AND therapy in the same session.
C. Supervision / Provider-Type Modifiers
Many Medicaid and commercial plans require:
- HP — Psychologist (Doctorate level)
- HO — Master’s level clinician
- HT — Supervised provider (intern, associate, trainee)
Missing these modifiers is one of the most common failures in behavioral health complex billing.
🖥️ 5. Telehealth Rules in Behavioral Health Complex Billing
Behavioral health is the largest telehealth service category in the U.S. However, the telehealth billing rules are extremely payer-specific.
Required elements for telehealth billing:
- POS 02 (telehealth) or POS 10 (home telehealth)
- Modifiers 95 or GT
- Provider must be licensed in the patient’s state
- Patient location documentation
- Consent for telehealth
- Platform security (HIPAA-compliant)
Behavioral health complex billing for telehealth also varies by Medicaid program—some states reimburse only certain codes or limit telehealth billing for supervised providers.
Behavioral health is the largest telehealth service category in the U.S. However, the telehealth billing rules are extremely payer-specific.
🛡️ 6. Prior Authorization Requirements in Behavioral Health
Behavioral health has more preauthorization requirements than primary care.
Common codes requiring authorization include:
- 90837 (60-minute psychotherapy)
- 90792 (comprehensive psychiatric evaluation)
- 90847 (family therapy)
- Psychological testing codes (96130–96139)
- MAT (Medication-assisted treatment)
- Partial hospitalization / IOP programs
Payers may require:
- Clinical notes
- Treatment plan
- Risk assessment
- Justification of medical necessity
Failure to meet these requirements results in retroactive denials, even months later.
❌ 7. Why Denials Are Higher in Behavioral Health Complex Billing
Behavioral health claims are denied at a significantly higher rate than standard medical claims.
Top reasons include:
❗ Missing modifiers (HP, HT, HO, 25, 59, 95)
❗ Time vs CPT mismatch
❗ Uncredentialed providers
❗ Incorrect POS for telehealth
❗ Invalid taxonomy codes
❗ Missing authorization
❗ Insufficient documentation
❗ Billing supervised providers incorrectly
Behavioral health denial management requires specialized knowledge, detailed worklists, and payer-specific correction strategies.
🏥 8. Supervision Rules and Provider-Type Restrictions
Behavioral health uniquely requires understanding provider roles:
✔ Providers who typically CAN bill:
- Psychiatry MD/DO
- Psychiatric NP
- Psychologist (PhD, PsyD)
- Licensed Clinical Social Worker (LCSW/LICSW)
- Licensed Professional Counselor (LPC/LPCC)
- LMFT
❌ Providers who often CANNOT bill:
- Associates
- Interns
- Residents
- Trainees
- Peer support
- Case managers
- Coaches
In behavioral health complex billing, incorrect billing under supervising providers can trigger fraud allegations—especially in Medicaid.
📊 9. Why Credentialing Is Especially Complex for Behavioral Providers
Credentialing and enrollment for behavioral health providers involves:
- State boards
- Medicaid specific enrollment portals
- CAQH roster maintenance
- Individual and group contracts
- Supervision-based limitations
- Taxonomy accuracy
Many states require separate credentialing for:
- Psychologists
- Therapists
- NPs
- Outpatient mental health clinics
Behavioral health complex billing fails when providers are not properly credentialed, leading to delayed payments or total claim rejections.
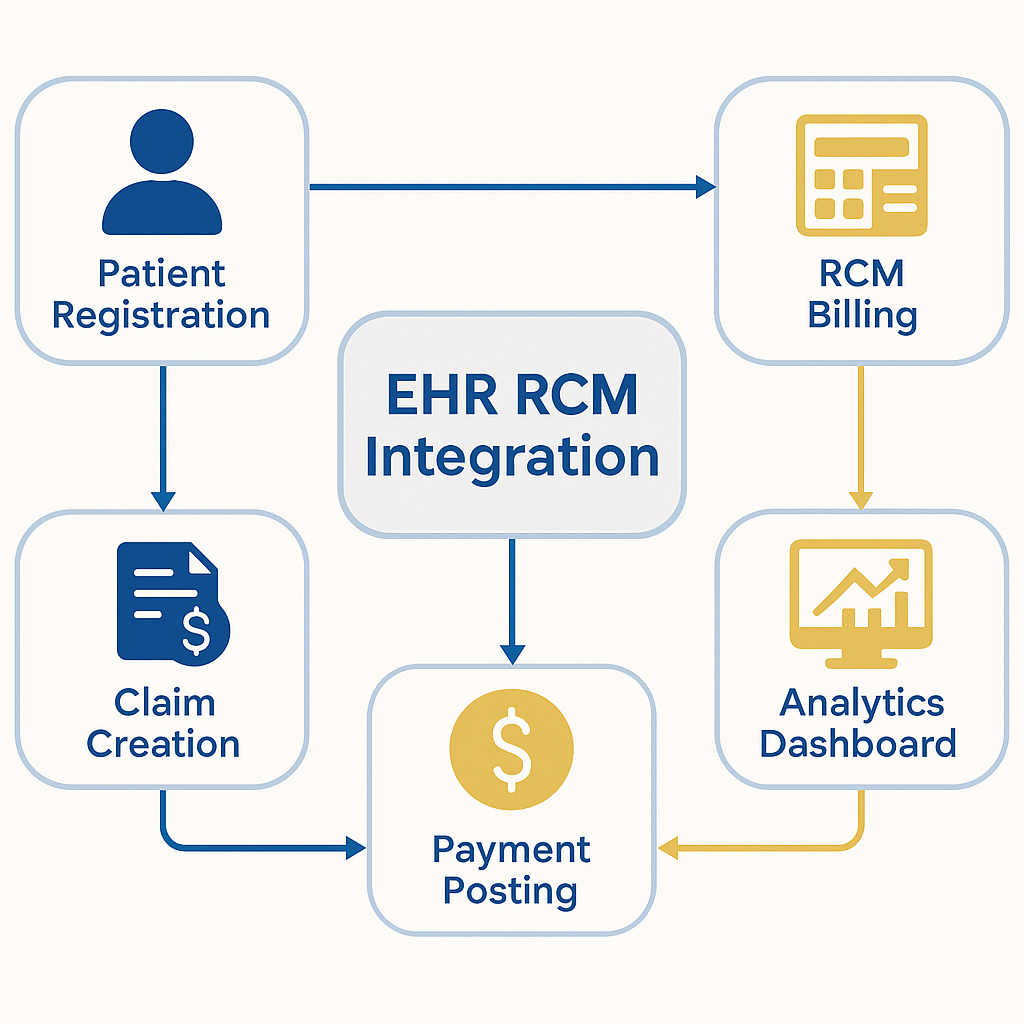
🔧 10. Best Practices for RCM Teams in Behavioral Health Complex Billing
To ensure clean claims and fast payment, RCM teams should implement:
✔ Payer-specific cheat sheets
✔ Standard documentation templates
✔ Audit workflows
✔ Telehealth compliance checklists
✔ Eligibility verification for every visit
✔ Monthly denial analytics
✔ Credentialing dashboard tracking
✔ Supervision logs
✔ Real-time billing alerts
✔ KPI monitoring (clean claim rate, denial rate, AR aging, 90837 approval rate)
Behavioral health complex billing requires a proactive, specialized approach—not generic billing.
🏆 11. Why Behavioral Health Practices Choose The Ashez Group
The Ashez Group, a Certified Woman-Owned RCM & Billing Company, specializes in:
- Psychiatric billing
- Therapy billing
- Behavioral telehealth billing
- Medication management claims
- Complex CPT coding
- HIPAA compliance
- Denial management
- Credentialing & enrollment
- Medicaid behavioral health billing
- Multi-state RCM solutions
Our behavioral health billing experts help reduce denials, improve provider revenue, and maintain compliance across multiple states.
We follow CMS Guidelines
Because behavioral health complex billing involves strict payer policies, RCM companies should reference federal standards like CMS.gov and HHS Telehealth requirements.
❓ 13. FAQ
Q1: Why is behavioral health billing more complex than medical billing?
Because it requires time-based coding, documentation-heavy notes, strict supervision rules, and modifier-specific billing.
Q2: What CPT code is most commonly denied?
90837 is the highest-denied code due to strict medical necessity requirements.
Q3: Can supervision-level providers bill insurance?
Only if the payer and state allow it, often with modifiers HP/HT.
Q4: Why does behavioral health documentation matter so much?
Because payers audit therapy sessions more aggressively than medical visits.icensed provider?
Depends — many states prohibit it unless explicitly allowed by payer.
Learn more about professional behavioral health billing solutions at The Ashez Group via our verified listings on GoodFirms, Clutch, and Alignable.